
- Prescription Assistance
- Free Rx Assistance Drug Cards Low/No Cost Health Care Programs
- Medicare Drug Coverage
- Medicaid and Childrens Health Insurance Programs (CHIP)
- Alzheimer's
- Blood Pressure
- Generic Medicine
- Healthy Pregnancy
- Heart Health
- Immunization
- Kidney Health
- Lung & Respiratory
- Men's Health
- Mental Health
- Multiple Sclerosis
- Women's Health
More Information
- Health Information Directory
- Drug Information Search
- Healthy Recipes
News Topics
- Drug Recalls
- Medical Association
- Prescription Drugs
- Pharmacy News
- Continuing Education
- Pharmacy Benefits Management
RxResource Home > Pharmacy Resources > Pharmacy Benefit Management

2441 Warrenville Road, Suite 610 Lisle, IL 60532-3642
Susan Fleming, Vice President, Marketing
Phone: (630) 577-4880
http://www.catamaranrx.com/
Catamaran offers a true alternative to the status quo in pharmacy benefit management. You don't have to choose between the scale and purchasing power of the largest providers and the flexibility and agility of smaller ones. We offer the best of both.
At Catamaran, we put your individual needs - and those of your members - at the center of our services. We connect pharmacists, doctors and caregivers with prescription data to improve health outcomes, offering the clinical intelligence, technology and scale to lower payer costs while improving member health.
- Pharmacy Resources
- What is a PBM?
- What Does a Benefits Manager Do?
- What To Do When You Can't Afford Your Medication

PBM Info from the FDA
- Pharmacy Benefit Management Companies (PBMs)
- The Influence of PBMs and HMOs on Prescription Drug Prices
- PBM Glossary
PBM News Articles
- Rankings - Best Pharmacy Coupons April 8, 2016
- Rankings - PBM Drug Rebates March 22, 2016
- PBM Rankings - Best Discount Drug Card June 9, 2012
- Top 10 PBM Companies - Rankings: Best Funded PBM June 8, 2012
- Wish List: 10 Things You Want From Your PBM November 29, 2011
- Important Links
- Prescription Assistance Programs
- Health Resources
- Healthy Living
- Terms of Use
- Privacy Policy
Website Administered by RxResource.org © 2024 RxResource

- Sustainability
- R&D/Clinical Trials
- Executive Roundtable
- Sales & Marketing
- Executive Profiles
- Market Access
- Patient Engagement
- Supply Chain
- Industry Trends
Scaling the Limits of Scale: The PBM Path to Value-Based Healthcare
Scale has its limits, as the nation’s two largest pharmacy benefit managers (PBM), Express Scripts and CVS Caremark, are discovering. Stephen Littlejohn reports.
Scale has its limits, as the nation’s two largest pharmacy benefit managers (PBM) are discovering. Express Scripts and CVS Caremark each process more than a billion prescriptions a year. That is not enough for big customers Anthem and Aetna. Both are likely to alter dramatically or not renew long-term contracts set to end in 2019 with the PBM behemoths.
PBM Optionality for Anthem, Aetna
Anthem and Aetna say they now have “optionality” because Cigna and Humana, which they are respectively acquiring, both have PBMs. That optionality goes well beyond the scale Aetna would enjoy as the fourth largest PBM. It can put the pharmacy benefit, integrated within each organization, on the path to value-based health care.
Both the Humana and Cigna PBMs align well with the quality and outcomes focus of value-based health care. Humana’s PBM primarily supports the company’s Medicare Advantage (MA) and Part D programs, with MA accountable care arrangements delivering better outcomes than traditional Medicare.
Meanwhile, Cigna has pioneered outcomes-based reimbursement arrangements with pharmaceutical manufacturers. Previously overseeing Cigna’s PBM was none other than Aetna CEO Mark Bertolini ; Cigna CEO David Cordani will serve as chief operating officer of the new Anthem.
In their sights is UnitedHealth Group (UHG), which brought its PBM business inside from Medco at the start of 2013, trigging Express Scripts’ anticipatory acquisition of Medco in 2012 . UHG says its OptumRx PBM focuses “ on connecting total condition spend and pharmacy’s impact across benefits ,” a process it calls “synchronization.”
More explicitly than Anthem, Aetna has said it will integrate Humana’s PBM, along with its “ growing health care services business ,” even characterizing it as an “ Optum-like business .”
Value beyond Scale
UHG’s Catamaran acquisition earlier this year, while adding scale, also significantly included Catamaran’s RxClaim processing platform. OptumRx plans to integrate the adjudication platform with its medical and pharmacy claims synchronization. UHG promises to create value “beyond the scale … resulting from integration,” by linking “demographic, lab, pharmaceutical, behavioral and medical treatment data” to encourage healthy decisions and improve compliance with pharmaceutical use and care protocols.”
In fact, the very tools used to leverage scale to get lower prices, such as formulary exclusions, can potentially work against reducing total costs. In securing a substantial discount from AbbVie for Viekira Pak, Express Scripts excluded Gilead’s Harvoni from its 2015 formulary. Viekira Pak is a four pill a day regimen to Harvoni’s adherence-friendly one pill for curing hepatitis C.
Not surprisingly, given their focus on overall costs, Aetna, Anthem, UHG and Cigna all included Harvoni on their formularies and do not publish exclusion lists like Express Scripts and CVS Caremark. Instead, they typically establish clinically based prior authorization criteria.
For the latest high-cost drugs to hit the market, Express Scripts is following the health plans on their value path. Instead of excluding one of two new anti-cholesterol drugs, known as PCSK9 inhibitors and list priced at $14,000 per year, it announced coverage for both this week .
As the health plans did with Harvoni, Express Scripts will implement rigorous prior authorization procedures. The company says it negotiated good pricing with Amgen for Repatha and with Sanofi and Regeneron Pharmaceuticals for Praluent, enabling it to cover both drugs. Perhaps it also heard from customers unhappy with price-driven drug exclusions.
Wanting More, Customers Become Competitors
Clearly, some very big customers – Aetna, Anthem and UHG – want something more than scale from traditional PBMs like Express Scripts and CVS Caremark. Beyond scale, they want a pharmacy benefit that contributes to reducing total costs through better outcomes, consistent with achieving overall value-based payment goals .
Building PBM paths to value-based health care for themselves, Anthem, Aetna and UHG will also sell against volume-based models like those of Express Scripts and CVS Caremark, and against health plans that fail to integrate pharmacy and medical claims for actionable intelligence.
Employers and the Limits of Scale
Their strategy blueprint could easily have come from the Harvard Business Reviewarticle “The Limits of Scale.” Hanna Halaburda and Felix Oberholzer-Gee argue that, when rapidly scaling companies neglect to take into account differences among their customers, performance declines. On that premise, they suggest how challengers and incumbents can take advantage of customer differences.
Among PBM customers with differences are employers, which provide health coverage for 147 million Americans . The National Business Coalition on Health is uneasy with the growing use of exclusionary formularies. It advises members to “base selection criteria for formularies on clinical outcomes to ensure that pharmaceutical costs do not decrease at the expense of rising medical costs.”
Employers are becoming more actively engaged in managing the pharmacy benefit, even developing their own formularies and negotiating directly with pharmacy retailers. Caterpillar’s Daren Hinderman told an NBCH panel last year, “I don’t want to have a conversation [with PBMs] on rebates; I want to have a conversation on how I can keep my employees more compliant with medications they need to stay healthy. We decide what’s best for our employees. It’s a transparent process.”
NBCH also urges members to “verify that pharmacy and medical benefits are aligned, and link data between the two in order to evaluate cost and outcomes across both types of benefits and the entire health-care spectrum, not just through the lens of pharmacy.” As Dr. Mark Fendrick of the University of Michigan Center for Value-Based Insurance Design told the NBCH panel , “I’d prefer to spend more on statins than on stents.”
Obstacles on PBM Value Path
Mapping the PBM path to value-based health care is one thing, building it is another. Aetna and Anthem still must face a gauntlet of government and legal reviews before they can complete their acquisitions and commence integrating the Humana and Cigna PBMs.
OptumRx must complete its integration of Catamaran, which in turn is still integrating the data platforms of its acquisitions . Furthermore, OptumRx and Catamaran both use different versions of the RxClaim platform and, for Catamaran, medical claims synchronization remains down the road (or path).
Meanwhile, the Catamaran acquisition has roiled a PBM industry where many participants use Catamaran’s RxClaim platform – including Cigna ! They were content to compete with Catamaran, despite using its technology. However, will they be similarly comfortable with OptumRx and UHG in the technology driver’s seat?
Much like UHG’s acquisition of Catamaran and its technology, Rite-Aid did the same when it acquired EnvisionRx . The PBM had previously acquired Laker Software , also a claims platform supplier for many PBMs. Again, the comfort question arises, in this case over Envision and Rite Aid as the drug retailer pursues its path to value-based health care via innovative alliances with health care providers.
Making the Laker and RxClaim platforms particularly valuable has been the PBM industry’s reliance on a hodge podge of decades-old, antiquated platform technologies. With each acquisition, scaling PBMs have patched together instead of invested in their platforms to maximize short-term synergies, at the cost of limited flexibility and lower efficiency.
PBMs Miss Technology Revolutions
Meanwhile, multiple revolutions have coursed through the systems development world since the PBM industry acquired its mainframes and data centers in the late 1980’ – early 1990’s. When relational databases followed soon thereafter, PBMs adopted them for after-the-fact data analysis, but not broadly for real time use with claims processing platforms, which now are antiquated and fragmented.
More recently, graphical user interfaces have greatly streamlined the programming of business intelligence applications. It is now easier for more people, more efficiently to translate their expertise into innovative systems. No longer must visionaries exclusively funnel their solutions through highly specialized programmers and coders. Now, the visionaries’ can become coders, their hands on the programming controls, unleashing new applications across the entire economy, including the PBM industry.
PBM Platform for Value-Based Health Care
One such visionary has developed a PBM solution for value-based health care. His name is Ravi Ika. “The solution is holistic, unlike that of any other existing PBM. It reduces overall pharmacy cost, converts specialty from ‘buy & bill’ to ‘authorize and manage,’ and lowers avoidable drug-impacted medical costs,” explains Ika.
Before turning his attention to the PBM industry, he created a comprehensive, integrated payer platform now provided by ikaSystems , which he founded to transform the payer operating model. Spanning all payer departments and business lines, it decreased administrative costs for health insurers by as much as 50% and reduced avoidable medical costs.
In 2013, Ika launched RxAdvance , a full service PBM, which similarly operates on an integrated, end-to-end platform – one designed specifically for value-based health care. Combining pharmacy, medical, and lab data, the platform – called PBM Collaborative Cloud– enables real-time engagement. This engagement occurs with physicians at the point of care, pharmacists at the point of sale, and patients via mobile cloud. It also engages payers clinical and pharmacy staff through their workflows.
Better decisions by these stakeholders – driven by platform-generated, actionable intelligence – can reduce avoidable drug-impacted medical costs, optimize utilization, facilitate better specialty drug management, and decrease overall pharmacy costs.
PBM Processes Reimagined
“We started with a clean slate,” observes Ika, who says he and his team reimagined PBM processes to streamline workflow before building the platform. Redefining the human role, they automated as much as possible while, on the other hand, increasing opportunities for engagement, what-if modeling, and informed decision-making. The platform also enables market and regulatory changes configurable by the business user, as well as system-driven compliance management.
Ika built the platform from the ground up using a unified data model . In information technology parlance, that means the platform’s standards are universal enough to encompass a large scope of data and types of data with high scalability.
In PBM language, the platform includes everything from pharmacy claim adjudication, formulary management, benefit design, enterprise reporting and analytics, to pharmacy network and rebate contracting, medication adherence and therapy management, specialty management, transparency, compliance, and adverse drug event management.
From Existing to Ideal Formularies
For example, the platform includes algorithm-driven artificial intelligence to manipulate, with plan sponsor engagement, the complex and interdependent variables associated with formulary management. Incorporating habitual member and prescriber utilization patterns, in addition to other data, it derives an ideal formulary with optimal financial and clinical outcomes. The system then maps a transition plan from an existing formulary. The platform also accommodates an unlimited number of formularies and supports real time dynamic modeling and changes coupled with full transparency.
Better Medication Therapy, Adherence Outcomes
For medication therapy management (MTM), the platform taps patient medical claims and disease conditions, against which the system overlays a prescription listing for easy use by prescribers. In addition, each new prescription triggers a dynamic analysis to determine patient eligibility for a comprehensive medication review (CMR), which the system prepopulates for efficient prescriber use.
After the CMR, RxAdvance advisors rely on system alerts to intervene with patients to ensure medication adherence. For high-risk patients, RxAdvance will install an electronic, patent-pending pill station at their residences and resupply it with disposable pre-filled pill trays.
Integrated with and wirelessly connected to the company’s platform, the device assists with monitoring adherence and vital signs. The company says the device has improved adherence to more than 93%, including patients with multiple chronic conditions who are taking an average of 15 medications a day.
The Centers for Medicaid and Medicare Services (CMS) recently underscored the PBM need for physician-led, point-of-care MTM capability when it announced a new Medicare Part D MTM model. Currently, highly fragmented PBM MTM relies on pharmacists “chasing” patients without closing the loop with prescribers, thus failing to secure meaningful health outcomes, according to Ika.
Ika points to the RxAdvance specialty management program as another example of his platform’s capabilities. As it does for MTM, the platform integrates prescriptions, medical claims and disease conditions to create an action plan for all stakeholders. Case managers use a dashboard to prioritize their outreach to patients, prescribers and pharmacists. Because the platform integrates medical, pharmacy and lab information, it helps facilitate appropriate utilization.
Risk Sharing
One of the hallmarks of an organization configured for value-based health care is its ability to share risk . The RxAdvance unified data model platform enables it to share risk for both pharmacy and avoidable drug-impacted medical costs. For pharmacy, it is prepared to assume both up and down side risk based on its cost management performance against a risk cap set below a national benchmark projected increase.
The company can also compute a baseline trend for avoidable drug-impacted medical costs using prior years’ medical claims data. RxAdvance and its client then set a target and, if the PBM lowers actual avoidable drug-impacted medical costs, it will share in the savings. According to Ika, this sort of risk sharing is unique in the PBM market.
Ika reports that RxAdvance is currently implementing full PBM services for three clients, replacing national PBMs. “The Collaborative PBM Cloud platform is making for a very smooth launch,” he notes.
RxAdvance has gotten a head start along the PBM path to value-based health care, scaling the limits of scale.
Stephen Littlejohn is President of Climb the Curve Communications. He can be reached at [email protected] and on Twitter @ClimbtheCurve . This article was originally posted on his website .

Understanding the Current State of M&A: Q&A with Cheryl Reicin
As the second half of 2024 begins, an industry expert discusses how mergers and acquisitions are trending in the pharma industry.

Embracing FSPs: Q&A with Jenny Denney
Pharmaceutical companies are seeing the benefits of being able to outsource entire functions through functional service providers.

Revitalizing Mature Pharma Brands: 5 Winning Strategies
Strategies that can help maintain and grow your market share. Plus how to adapt to new competitive pressures and evolving customer needs.

A Case for Payer Engagement and Participation in Clinical Research
Collaboration can make commercialization processes efficient and effective.

Targeted Pre-Launch Scientific Outreach: Q&A with Dan Rizzo
Rizzo discusses Veeva’s latest findings on how life sciences companies are utilizing this strategy to speed up uptake of new treatments.
2 Commerce Drive Cranbury, NJ 08512
609-716-7777

- Today's news
- Reviews and deals
- Climate change
- 2024 election
- Newsletters
- Fall allergies
- Health news
- Mental health
- Sexual health
- Family health
- So mini ways
- Unapologetically
- Buying guides
Entertainment
- How to Watch
- My watchlist
- Stock market
- Biden economy
- Personal finance
- Stocks: most active
- Stocks: gainers
- Stocks: losers
- Trending tickers
- World indices
- US Treasury bonds
- Top mutual funds
- Highest open interest
- Highest implied volatility
- Currency converter
- Basic materials
- Communication services
- Consumer cyclical
- Consumer defensive
- Financial services
- Industrials
- Real estate
- Mutual funds
- Credit cards
- Balance transfer cards
- Cash back cards
- Rewards cards
- Travel cards
- Online checking
- High-yield savings
- Money market
- Home equity loan
- Personal loans
- Student loans
- Options pit
- Fantasy football
- Pro Pick 'Em
- College Pick 'Em
- Fantasy baseball
- Fantasy hockey
- Fantasy basketball
- Download the app
- Daily fantasy
- Scores and schedules
- GameChannel
- World Baseball Classic
- Premier League
- CONCACAF League
- Champions League
- Motorsports
- Horse racing
New on Yahoo
- Privacy Dashboard
UnitedHealth to buy pharmacy benefit firm Catamaran for $12.8 billion
By Sneha Banerjee (Reuters) - Health insurer UnitedHealth Group Inc agreed to buy Catamaran Corp in a deal worth about $12.8 billion to boost its pharmacy benefit business as it competes with bigger rivals such as Express Scripts Holdings Co . Pharmacy benefit managers (PBM) administer drug benefits for employers and health plans and run large mail order pharmacies, helping them get better prices from drugmakers. As employers look to cut prescription costs on expensive drugs, the deal with Catamaran will give UnitedHealth's pharmacy benefits unit, OptumRx, the scale to negotiate favorable prices from pharmacy companies. U.S. drug prices rose 12 percent in 2014 due to a new treatment for hepatitis C that cost more than $80,000 but cured almost all recipients with few side effects. Another new class of drugs, to treat high cholesterol, is expected to hit the market in 2015 and has insurers worried about drug costs this year as well. The purchase of Catamaran will increase UnitedHealth's market share to 15 percent to 20 percent of the people who receive their drug benefits through pharmacy benefit managers, BMO Capital Markets analyst Jennifer Lynch said in a research note. With a combined 1 billion scripts annually, UnitedHealth will be about the same size as current industry number two, CVS Health Corp , she added. Catamaran was formed after SXC Health Solutions and PBM Catalyst Health Solutions merged in 2012. UnitedHealth's offer of $61.50 per share represents a premium of 27 percent to Catamaran's Friday close on the Nasdaq. Catamaran's stock was trading at $60.01 premarket on Monday, while UnitedHealth was up nearly 4 percent. The deal "makes sense to us, but admittedly came much earlier than we expected," Jefferies analyst Brian Tanquilut said in a research note. "We had always viewed Catamaran as a compelling asset for companies looking for scale in the PBM sector such as Optum or Walgreens but expected Catamaran to grow the business much further before pursuing a sale." He added that the offer seemed adequate and he did not expect competing bids at this point. The deal value is based on Illinois-based Catamaran's total diluted shares outstanding as of Dec. 31. The transaction is expected to close in the fourth quarter of 2015 and add about 30 cents per share to UnitedHealth's profit in 2016, the companies said. Catamaran Chief Executive Officer Mark Thierer will be CEO of OptumRx and OptumRx CEO Timothy Wicks will become president. (Additional reporting by Caroline Humer in New York; Editing by Savio D'Souza, Saumyadeb Chakrabarty and Meredith Mazzilli)
Recommended Stories
Women in their 50s are scoring fall fashion finds at these 4 retailers.
Shop just a handful of sites (yep, Amazon made the list) to nail a stylish, affordable wardrobe upgrade.
What a bigger-than-expected Fed rate cut would mean for the stock market
Recent market history shows the Federal Reserve typically only starts interest cuts with 50 basis point reductions when the economy is significantly weakening.
WNBPA, players condemn commissioner Cathy Engelbert over interview about race, Caitlin Clark-Angel Reese rivalry
The WNBA players union and several players slammed the commissioner on Tuesday after her appearance on CNBC.
College Football Playoff Picture: Here's what the 12-team bracket looks like after Week 2
The first iteration of the 12-team College Football Playoff is only months away. After two weeks of action, the field is filled with SEC teams.
Mortgage and refinance rates today, September 12, 2024: Rates fall after CPI news
These are today's mortgage and refinance rates. The national 30-year and 15-year rates have hit their lowest points in months. Lock in your rate today.
What credit card users need to know if the Fed cuts rates in September
The Fed may soon cut interest rates. Here’s why you should take control of your credit card debt now.

Where does Notre Dame's stunning loss fall among the biggest upsets in college football history?
Northern Illinois defeated Notre Dame in South Bend as 28.5-point underdogs.
A 2024 Ford Mustang GT with a Whipple-sourced 810-hp is a really good time
Autoblog chats to a hardcore Mustang fan and takes a spin in his 2024 Mustang with Ford Performance's new Whipple supercharger package.
Anne Hathaway's joined the legions of fans sporting these $50 Birkenstock slides
Stay comfortable and look stylish in these A-list-approved sandals.
Angel Reese announces she's out for season with injury, currently has most rebounds in WNBA history
Angel Reese's record-setting rookie season is over two weeks before anyone expected.
Deion Sanders wonders why Travis Hunter and Shedeur Sanders didn't get more Week 1 recognition
Colorado beat FCS school North Dakota State 31-26 in Week 1.
MLB suspends Rays pitcher Edwin Uceta 3 games for throwing at Phillies' Nick Castellanos
Rays manager Kevin Cash also got a one-game ban for the incident.
Asked & Answered: Steelers, Bengals have QB questions; Kyler Murray, Minnesota offer answers
Do the Steelers turn to Justin Fields or Russell Wilson? And is Joe Burrow's wrist cause for concern?
Oprah's fave sneakers — Vionics — are on sale, from $25 (that's over 60% off)
Fall footwear that looks as good as it feels, with a starry seal of approval — all at a massive discount.
Lucid CEO: New midsize cars, EV tech make Lucid a long-term play like Tesla and Amazon
EV maker Lucid Motors revealed new information today about its upcoming Gravity SUV at its Technology & Manufacturing Day, along with updated delivery numbers for 2024 and a glimpse of its upcoming midsize SUV.
Nebraska is almost back & the House Case settlement is in jeopardy | College Football Enquirer
What is Matt Rhule building at Nebraska? Dan Wetzel, Ross Dellenger and SI's Pat Forde look back at the impressive victory for the Cornhuskers this weekend. They evaluate the job head coach Matt Rhule has done rebuilding the program, and project if they have a shot finish at the top of the Big Ten in 2024.
Ricky Pearsall shooting: Defendant's lawyer hopes video of 'extended struggle' can nullify attempted murder charge
New surveillance footage of the incident has reportedly been unearthed.
2025 Ford Mustang 60th Anniversary adds Brittany Blue to the palette
Brittany Blue is joining as one of the possible colors for the Mustang's 60th Anniversary Package.
Disney 'is playing hardball' with DirecTV over 'skinnier' bundles. Here's what's at stake.
A contract dispute between Disney and DirecTV continued into its second week on Monday as subscribers remain without access to ESPN, ABC, and other Disney-owned channels.
Turn your car into a comfortable camper for less than $100
Just because you can spend thousands of dollars converting a vehicle into something you can comfortably sleep in doesn’t mean you should.

Catamaran officially becoming OptumRx
Effective October 1, 2015, Catamaran, Caterpillar's pharmacy benefit manager (PBM), will change its name to OptumRx. This PBM branding change doesn't impact design or coverage under our prescription drug plan.
Plan participant materials mailed from Catamaran will start to show OptumRx branding. Catamaran ID cards will continue to be accepted at pharmacies and won't need to be replaced. The processing information and phone number listed on the cards are not changing.
Nothing! It's a name change only. If you're a plan participant, you can continue to access your pharmacy records and drug information using the same website ( mycatamaranrx.com ) and mobile app (OptumRx/CatamaranRx in your mobile device's app store) as always. You may also access prescription drug benefit information at benefits.cat.com .
Cookie Policy




IMAGES
VIDEO
COMMENTS
Catamaran Corporation (formerly SXC Health Solutions) is the former name of a company that now operates within UnitedHealth Group's OptumRX division (since July 2015). It sells pharmacy benefit management and medical record keeping services to businesses in the United States [3] and to a broad client portfolio, including health plans and employers. [4] ...
Highlighting the new focus, Mark Thierer, Catamaran's chairman and CEO, will become CEO of OptumRx. One immediate task will be to convert the UnitedHealthcare national accounts that are not using OptumRx. Integration risk should be minimal, because OptumRx is reportedly already using Catamaran's RxClaim technology platform.
OptumRx was an early champion of Synchronization and now, with the combination of OptumRx and Catamaran, we will take it to the next level together. Specifically, we are focused on: Connected Care - Blending health systems, programs and people to address the complex needs of each consumer. Connected Engagement - Surrounding consumers at ...
Welcome to RxClaim Web This site allows employers and plan sponsors to manage their members' pharmacy benefits. Please sign in using your MSID/One Healthcare ID credentials.
Summary. Catamaran offers a true alternative to the status quo in pharmacy benefit management. You don't have to choose between the scale and purchasing power of the largest providers and the flexibility and agility of smaller ones. We offer the best of both. At Catamaran, we put your individual needs - and those of your members - at the center ...
But Thierer pointed out that most of the PBMs use Catamaran's RxClaim system -- "We have 5x market share on the technology side," said Thierer -- and Catamaran has been careful not to poach its ...
Furthermore, OptumRx and Catamaran bothuse different versions of the RxClaim platform and, for Catamaran, medical claims synchronization remains down the road (or path). Meanwhile, the Catamaran acquisition has roiled a PBM industry where many participants use Catamaran's RxClaim platform - including Cigna! They were content to compete with ...
OptumRx must complete its integration of Catamaran, which in turn is still integrating the data platforms of its acquisitions [25]. Furthermore, OptumRx and Catamaran bothuse different versions [26] of the RxClaim platform and, for Catamaran, medical claims synchronization remains down the road (or path).
We go beyond what a traditional pharmacy benefit manager offers. Connected with the power of Optum, we are uniquely positioned with differentiated capabilities to address your biggest challenges. There are more than 200,000 people focused on fundamentally transforming how health care is accessed, delivered and paid for.
By Sneha Banerjee. March 30, 2015. By Sneha Banerjee (Reuters) - Health insurer UnitedHealth Group Inc agreed to buy Catamaran Corp in a deal worth about $12.8 billion to boost its pharmacy ...
Dive Brief: Once UnitedHealth's $12.8 billion acquisition of pharmacy benefits manager (PBM) Catamaran closes, the insurer it will become the third largest PBM in the U.S. In terms of size, Express Scripts Holding Co. and CVS Health Corp. are the numbers one and two PBMs, respectively. The acquisition of Catamaran will provide UnitedHealth ...
OptumRx and Catamaran combine to strengthen pharmacy benefit services OptumRx® and Catamaran® have joined forces to deliver enhanced pharmacy benefit services and a better health care experience for members. Your prescription claims will continue to be processed quickly and accurately, and your pharmacy benefits will not change. Below are
Effective October 1, 2015, Catamaran, Caterpillar's pharmacy benefit manager (PBM), will change its name to OptumRx. This PBM branding change doesn't impact design or coverage under our prescription drug plan. Plan participant materials mailed from Catamaran will start to show OptumRx branding. Catamaran ID cards will continue to be accepted at ...
UnitedHealth Group, the nation's largest insurer, on Monday said it would acquire Catamaran, the country's fourth-largest pharmacy benefits manager, for $12.8 billion. Under terms of the deal, Schaumburg, Illinois-based Catamaran will merge with OptumRx, the drug management division of UHG's highly profitable technology and services subsidiary Optum.
Cigna recently decided it will not transition its commercial customers to the RxClaim processing platform. Accordingly, the 15 Cigna commercial clients currently on RxClaim will transition to Argus as of June 1, 2015. When processing Cigna commercial customer claims, you should continue to use the updated RxBIN (017010) and PCN information that appears on the customer's ID card. As of June 1 ...
Pharmacy - Catamaran Submitting 2016 Pharmacy Claims Only. All 2016 pharmacy claims should be directed to Catamaran at 877-235-2017 or www.mycatamaranrx.com. Mercy Health Employees (Toledo & Lorain) Pharmacy - Catamaran; Summary of Benefits and Coverage; Customer Relations;
Rxclaim is a Trademark by Catamaran LLC, the address on file for this trademark is 2441 Warrenville Road Suite 610, Lisle, IL 60532. Trademark Introduction: ... Catamaran Inc. Corporation: 1st New Owner After Publication: Texas · United States: 2441 Warrenville Road Lisle, IL 60532 : Sxc Health Solutions, Inc.
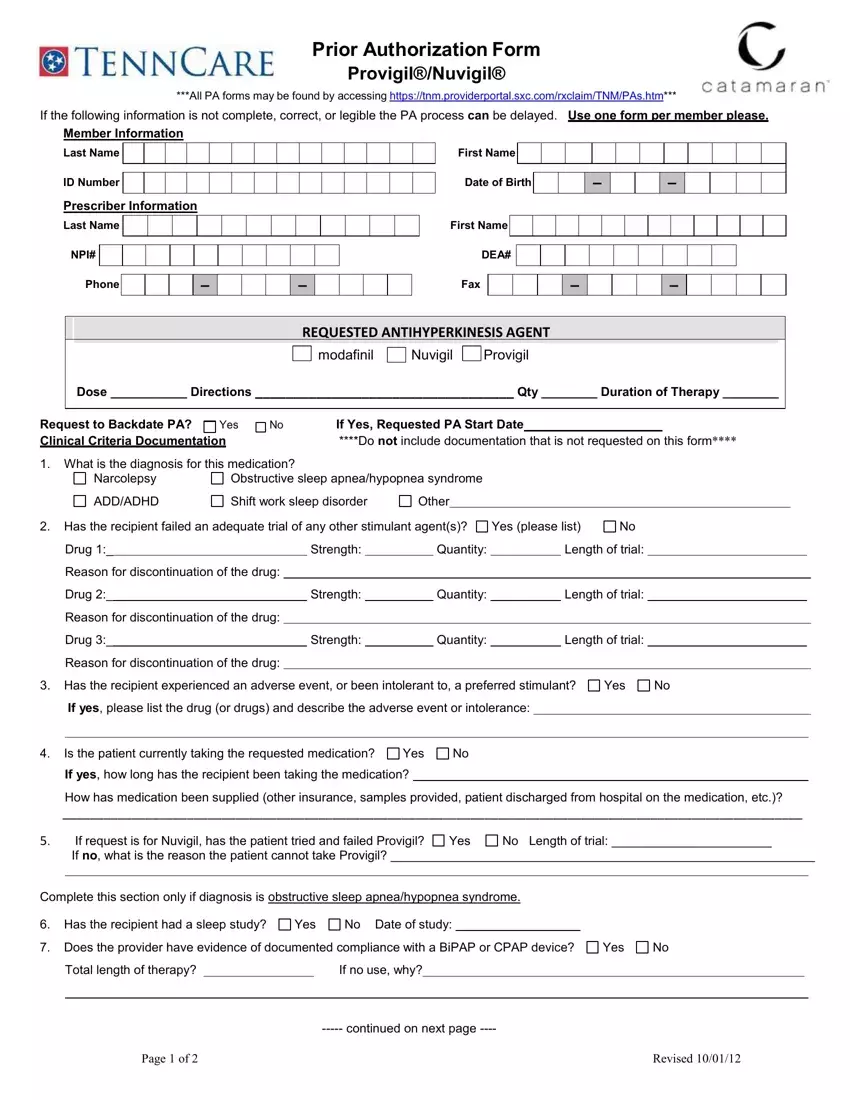
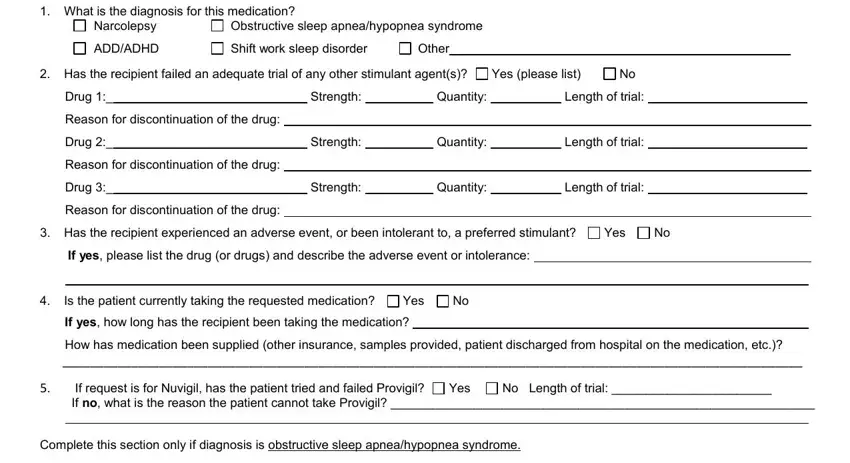
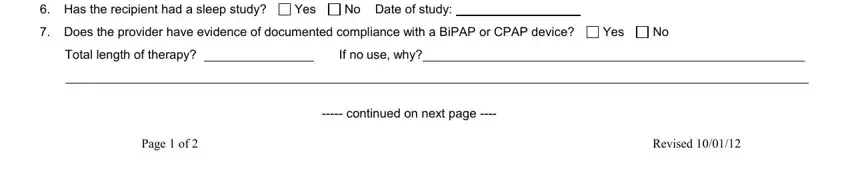
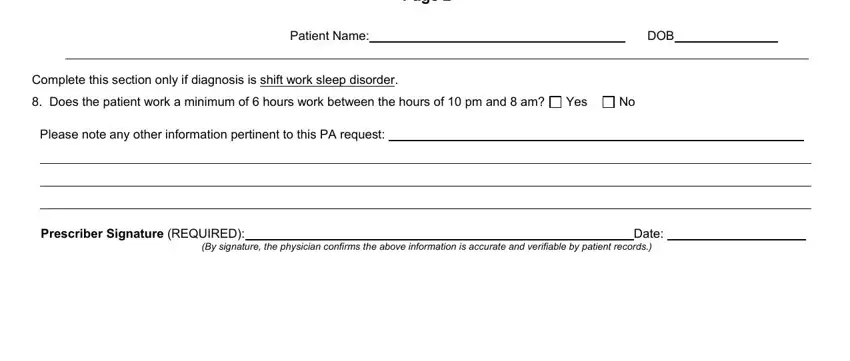
Catamaran Prior Auth Form - Fill Out and Use This PDF. The Catamaran Prior Authorization Form for Provigil®/Nuvigil® is a specialized document required to obtain prior approval from insurance providers before certain medications can be dispensed. This form must be filled out with precise member and prescriber information, including details about the requested medication, to facilitate the ...
Highlighting the new focus, Mark Thierer, Catamaran's chairman and CEO, will become CEO of OptumRx. One immediate task will be to convert the UnitedHealthcare national accounts that are not using OptumRx. Integration risk should be minimal, because OptumRx is reportedly already using Catamaran's RxClaim technology platform.
Tambov (UK: / t æ m ˈ b ɒ f / tam-BOF, [9] US: / t ɑː m ˈ b ɔː f,-ˈ b ɔː v / tahm-BAWF, - BAWV; [10] [11] [12] Russian: Тамбов, IPA:) is a city and the administrative center of Tambov Oblast, central Russia, at the confluence of the Tsna and Studenents rivers, about 418 km (260 mi) south-southeast of Moscow.With a population of 261,803 as of 2021, Tambov is the largest city ...
OKTMO ID. 68000000. Official languages. Russian [10] Website. www.tambov.gov.ru. Tambov Oblast (Russian: Тамбо́вская о́бласть, romanized: Tambovskaya oblastʹ) is a federal subject of Russia (an oblast). Its administrative center is the city of Tambov. As of the 2010 Census, its population was 1,091,994.
Administrative divisions of Tambov Oblast. with 8 selsovets under the district's jurisdiction. with 6 selsovets under the district's jurisdiction. with 13 selsovets under the district's jurisdiction. with 8 selsovets under the district's jurisdiction. with 14 selsovets under the district's jurisdiction.
Znamensky District (Russian: Знаменский райо́н) is an administrative and municipal district (), one of the twenty-three in Tambov Oblast, Russia.It is located in the southwestern central part of the oblast.The district borders with Tambovsky District in the north, Sampursky District in the east, Tokaryovsky District in the south, and with Morshansky District in the west.